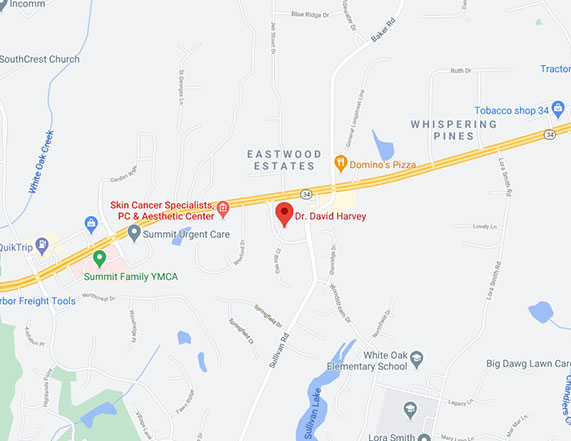
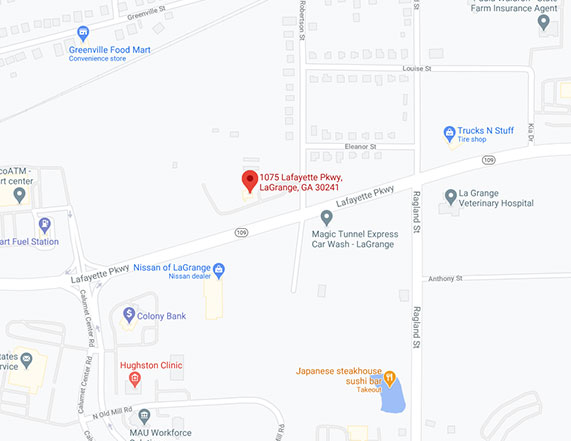
Conveniently located to serve Newnan, Peachtree City and LaGrange
Click here to jump to:
Newnan Melanoma
WHAT IS MALIGNANT MELANOMA?

Malignant Melanoma is known as the most fearsome type of skin malignancy. Melanoma accounts for less than 5% of skin cancer cases but causes a large majority of skin cancer deaths. In fact, it is estimated that 9,480 people will die of melanoma in 2013.
The American Cancer Society estimates that about 76,690 new melanomas will be diagnosed in the United States during 2013. From 1970 to 2009, the incidence of melanoma increased by 800 percent among young women and 400 percent among young men.
Melanoma is more than 10 times more common in whites than in African Americans. It is slightly more common in males than in females. The lifetime risk of getting melanoma is about 2% (1 in 50) for whites, 0.1% (1 in 1,000) for blacks, and 0.5% (1 in 200) for Hispanics. The risk for each person can be affected by a number of different factors, which are described below.
RISK FACTORS FOR DEVELOPMENT
Ultraviolet (UV) light exposure
Ultraviolet (UV) radiation is thought to be a major risk factor for most melanomas. Sunlight is the main source of UV radiation, which can damage the genes in your skin cells. Tanning lamps and booths are also sources of UV radiation. People with excessive exposure to light from these sources are at greater risk for skin cancer, including melanoma. Statistically, 86 percent of melanomas can be attributed to exposure to ultraviolet (UV) radiation.
The amount of UV exposure depends on the intensity of the radiation, length of time the skin was exposed, and whether the skin was protected with clothing and sunscreen.
The nature of the UV exposure may play a role in melanoma development. Many studies have linked the development of melanoma in the trunk, legs, and arms to frequent sunburns (especially in childhood). The fact that these areas are not constantly exposed to UV light may also be important. Some experts think that melanomas in these areas are different from those on the face and neck, where the sun exposure is more constant. And different from either of these are melanomas that develop on the palms, soles, nails or internal surfaces such as the mouth and vagina, where there has been little or no sun exposure.
Moles (Multiple or Atypical)
A nevus (the medical name for a mole) is a benign (non-cancerous) melanocytic tumor. Moles are not usually present at birth but begin to appear in children and teenagers. Most moles will never cause any problems, but a person who has many moles is more likely to develop melanoma.
A dysplastic nevus, or atypical mole, is a type of mole that particularly increases a person’s risk of melanoma. Dysplastic nevi (nevi is the plural of nevus) often look a little like normal moles but also look a little like melanoma. They can appear in areas that are exposed to the sun as well as those areas that are usually covered, such as the buttocks and scalp. They are often larger than other moles.
A small number of dysplastic nevi may develop into melanomas. But most dysplastic nevi never become cancerous, and many melanomas seem to arise without a pre-existing dysplastic nevus (1/3 rd of the time melanoma lesions originate in previously normal nevi).
Dysplastic nevi often run in families. If you have family members with many dysplastic nevi you have about a 50% chance of developing these nevi. Someone with 1 or more dysplastic nevi and with at least 2 close relatives with melanoma has a 50% or greater risk of developing melanoma.
Lifetime melanoma risk is estimated to be between 6% and 10% for those with many dysplastic nevi (sometimes referred to as dysplastic nevus syndrome). People with this condition should have very thorough periodic skin exams at our office. In some cases, full body photographs are taken at regular intervals to help the us recognize which moles are changing and growing. We recommend that patients be taught to do monthly skin self-exams and be counseled about sun protection tips.
Moles present at birth are called congenital melanocytic nevi. The lifetime risk of getting melanoma for people with congenital melanocytic nevi has been estimated to be between 0 and 10%, depending on the size of the nevus. People with very large congenital nevi have a greater risk, while the risk is smaller for those with small nevi. Congenital nevi are sometimes removed by surgery so that they do not have a chance to become cancerous. Advice on removing a congenital nevus is influenced by several factors including its size, location, color, and texture. We recommend that congenital nevi that are not removed should be examined at regular intervals.
The chance of any single mole turning into cancer is very low. However, anyone with lots of irregular or large moles has an increased risk for melanoma.
Learn the “ABCDE” Rule.

Melanoma lesions can be identified by the “ABCDE” rule. In essence this refers to skin lesions which are Asymmetric, have Border irregularity, develop a multitude of skin Colors, have a Diameter greater than 6mm, or are Evolving or changing. The earliest sign of a melanoma is itching. Moles or freckles which bleed, are tender or grow rapidly should also be evaluated by a dermatologist.
- A = Asymmetry of a mole
- B = Border irregularity of a mole
- C = Multiple Colors to a mole
- D = Diameter greater than 6mm (Pencil Eraser)
- E = Evolving Mole (Enlarging, Itching, Bleeding)
Fair skin, freckles, and light hair
The risk of melanoma is more than 10 times higher for whites than for African Americans. This is because skin pigment has a protective effect. Whites with red or blond hair or fair skin that freckles or burns easily are at increased risk. Red-haired people have the highest risk.
Related
Content
Patient
Review
“From the moment I walked in the door until I left … total excellence! I went in with a few spots that had me concerned and turned out that one of them was indeed skin cancer. I had to have it surgically removed and I was very concerned and nervous, being that is was JUST below my eye. The staff was very friendly, personable and above all professional. Dr. Harvey, AMAZING! Very much cares about the patient in front of him. He listens and explains.
Just 16 days post op, I AM VERY PLEASED with the surgery site. I firmly believe that within 3-6 months, you will not be able to tell, all thanks to DR. Harvey. Like I said, he is amazing.
I highly recommend him to anyone in need of dermatology care.”
by LT
Family History
Your risk of melanoma is greater if 1 or more of your first-degree relatives (mother, father, brother, sister, child) has been diagnosed with melanoma. Around 10% of all people with melanoma have a family history of melanoma.
The increased risk may be due to a shared family lifestyle of frequent sun exposure, a family tendency to have fair skin, or a combination of both factors. It may also be due to inherited gene changes (mutations) in a family. Gene mutations have been found in anywhere from about 10% to 40% of families with a high rate of melanoma. Most experts do not recommend genetic testing in these families at this time. Rather, they advise that people with a strong family history of melanoma do the following:
- have regular skin exams by a board certified dermatologist
- perform self skin examinations on a monthly basis
- employ sun protection measures
Personal History
A person who has already had melanoma has an increased risk of getting melanoma again. About 5% to 10% of people with melanoma will develop a second one at some point.
Immune suppression
People who have been treated with medicines that suppress the immune system, such as organ transplant patients, have an increased risk of developing melanoma.
Age
Although melanoma is less related to aging than most other cancers, it is still more likely to occur in older people. But this is one of the few cancers that is also found in younger people. In fact, melanoma is one of the most common cancers in people younger than 30, especially women in the younger age groups. Melanoma that runs in families may occur at a younger age.
Gender
Men have a higher rate of melanoma than women.
Genetics (Xeroderma pigmentosum)
Xeroderma pigmentosum (XP) is a rare, inherited condition resulting from a defect in an enzyme that normally repairs damage to DNA. People with XP have a high risk for developing both melanoma and basal cell and squamous cell skin cancers at a young age. Because people with XP are less able to repair DNA damage caused by sunlight, they can develop many cancers on sun-exposed areas of their skin
What are the various types of melanoma?

There are five types of melanoma with the prognosis being dependent not on the size of the lesion but on the depth into the skin that it penetrates. The major subtypes of melanoma include: Superficial Spreading type, Lentigo Maligna, Desmoplastic Melanoma, Acral Lentiginous Melanoma and Nodular Melanoma. Melanoma lesions which are flat and superficial in the skin can sometimes remain so for many years. These types of melanoma have a better survival and cure rate than those which penetrate deeply into the skin.
WHAT ARE SOME USEFUL TIPS REGARDING MELANOMA?

Melanoma can be diagnosed by routine physical examinations and noting if you have a first degree relative have a history of unusual moles or melanoma. A biopsy or sampling of the skin lesion will usually occur if melanoma or premelanoma (atypical nevus) is though to be present.
Our providers may also recommend total body photography or dermatoscopy (magnifying the skin) to detail the most earliest changes of your moles. Through pattern recognition, and noting any changes, your doctor can keep accurate records and make sure that no abnormal changes develop in your moles. Other more recent techniques to evaluate moles include ultrasound studies, computer generated analysis of moles, and spectroscopy.
Melanoma Patients Information Page – an excellent source for the latest treatments available for melanoma patients and a list of support groups. http://www.mpip.org.
WHAT ARE THE TREATMENTS AVAILABLE FOR MALIGNANT MELANOMA?
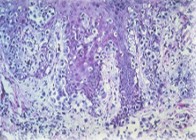
Melanoma – under the microscope
The treatment of malignant melanoma is surgical removal of the lesion with an appropriate margin of normal skin. In some instances, lymph node removal, radiation treatment or chemotherapy are utilized but these treatments are usually reserved for melanoma which may have spread internally. Melanoma can also be assessed by other techniques such as PET Scans which can assess invasive malignancy or lymph node scintigraphy which can identify the sentinel lymph node. Follow up total skin exams, once a diagnosis of melanoma has been made, should be performed every 3 to 6 months. Ocular exams such as the Optomap to assess the retinal background should also be performed.
For more information on malignant melanoma or to set up a consultation, click here. Thank you and we look forward to helping you.