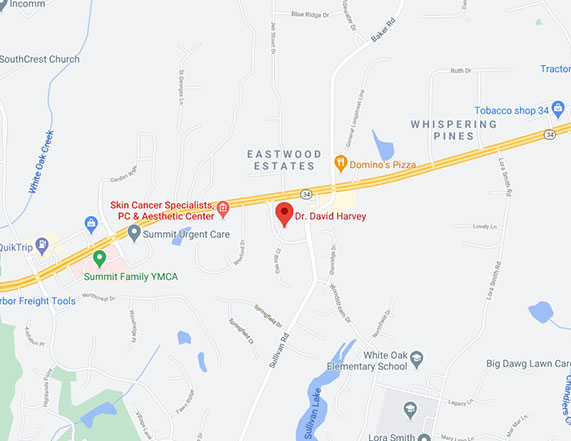
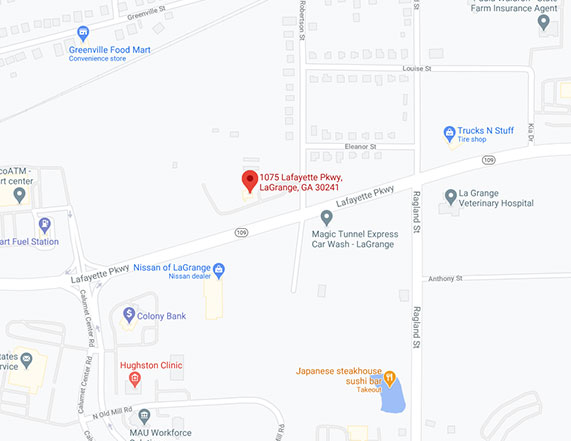
Conveniently located to serve Newnan, Peachtree City and LaGrange
Click here to jump to:
Newnan STD Treatment

VENEREAL WARTS (HPV) & HERPES SIMPLEX- 2
The human papilloma virus (HPV) is responsible for causing genital warts in the anus and genital area. More than 80 different specific types of HPV DNA have been identified. 45 of these can affect genital skin. The incidence of HPV infection has risen over the past three decades. An estimated 30 to 50% of sexually active adults in the United States are infected with HPV, making it the most common viral STD. However, only one to two percent of the same population has clinically apparent warts. The treatment for HPV can be difficult for some patients. Destructive means such as liquid nitrogen is most popular. Other new therapies, including Aldara™ Cream, which is an immunomodulator, or Condylox™ gel, have been useful in the treatment of resistant lesions. In areas that are extremely resistant to treatment, providers are sometimes ablate the warts with a carbon dioxide laser. As genital warts can cause one to develop carcinoma of the cervix or penis, it is important that our providers examine infected patients and their partners for non healing lesions. If one has both a non healing lesion on the genitals and a personal history of venereal warts, then it is important that this non healing lesion be biopsied to rule out malignancy.
WHAT ARE THE SIGNS THAT ONE HAS CONTRACTED HPV?
Warts are clinically apparent as flesh colored papules that erupt on the skin of the genital or perianal area. They can range in size from 1 mm in diameter to very large growths. One-third of women with external venereal warts also have internal vaginal and/or rectal warts, and, thus, need a gynecologic exam. Venereal warts usually do not have any symptoms, but can occasionally they can bleed or cause pain.
HOW CONTAGIOUS IS THE HPV VIRUS?
Little is known about the transmission of HPV. Risk factors for acquiring the virus include numerous sexual partners, frequent sexual intercourse, and the presence of warts in a co infected sexual partner. Men have been found to have an increased risk developing venereal warts if they fail to wear condoms. Although condoms reduce the transmission of HPV, their use it does not eliminate it completely.
Related
Content
Patient
Review
“There were no issues and everyone was very professional and attentive. Thank you!”
by Anonymous
IS HPV CURABLE?
Unfortunately, total eradication of this virus is not possible. Approximately 10 to 30% of venereal warts spontaneously resolve within three months. Removal of viral lesions, in theory, should reduce the likelihood of viral transmission, but this has not been proven scientifically.
HOW ARE GENITAL WARTS TREATED?
As mentioned above, treatment can be a difficult process. The most effective treatment modalities include liquid nitrogen which causes inflammation and the body to control and sequester the wart virus. Other therapeutic modalities include: surgical excision, laser treatment or acid. The choice of treatment utilized should be decided by the provider and the patient because there are several factors such as number and size of lesions which come into play. The newest treatment option for HPV is a drug called Imiquimod (Aldara™). Imiquimod is formulated as a topical cream preparation. It is designed to stimulate one’s immune system by stimulating the chemical protein known as interferon alpha, which has a negative effect on HPV. Initial studies have shown that this treatment is effective in 30% to 50% of patients. Imiquimod has been found to work better in women than in men. Please remember that many treatments are sometimes necessary for HPV control and that recurrence rate is high. Hopefully, in the near future we shall, see an effective cure. Currently, there is also a vaccine which is recommended for young female patents. Gardisil™ is a vaccine indicated in girls and women 9 to 26 years of age for the prevention of cervical cancer, precancerous or dysplastic lesions, and genital warts caused by human papillomavirus (HPV) Types 6, 11, 16, and 18
WHAT CAN ONE EXPECT DURING HPV TREATMENT?
Many of the modalities discussed above do cause temporary discomfort, i.e., redness, blistering, pain, can be seen. Recurrences occur most frequently during the first three months after therapy has been initiated. As previously mentioned, infected women, should have a full pelvic and cervical examination, because they have an increased risk of carcinoma of the cervix. Men should be examined for dysplasia (precancer or cancer) of the penis. Transmission of HPV during pregnancy may occur in infants who can, if mom has active disease during delivery, can acquire HPV virus in their throat and genital area without a previous history of sexual abuse.
SHOULD YOU CONTACT PAST PARTNERS?
Yes, because of the slight increased risk of cancer which can occur in both females and males. Examination of previous partners is advised. Education is the only way to reduce the risk of spreading HPV to other people. Because the HPV virus can lie dormant for many years, there is no way to know which sex partner gave you the infection. It is, therefore, sometimes difficult to try to blame a particular partner for giving you the infection. Remember the following:
- Refrain from sexual activity until three negative check ups are performed. Condoms are not completely protective.
- An OB/GYN Evaluation or Pap Smear to look for atypical cells
- Biopsy non responding lesions
- Regular follow up visits every two to four weeks to optimize your chances for wart eradication.
HERPES SIMPLEX VIRUS TYPE 2 (HSV-2)
Infection with HSV-2 usually results in sores on the buttocks, penis, vagina, or cervix, beginning two to twenty days after contact with an infected person. Sexual intercourse is the most frequent means of getting the infection. The virus affects anywhere between five and twenty million people, up to 20% of all sexually active adults in the United States.
Both primary and repeat attacks can cause symptoms from a minor rash to painful sores to a burning sensation with urination. HSV-2 may also occur in other locations, but usually the rash develops below the waist.
As with Type 1, sites and frequency of repeated bouts vary. The initial episode can be so mild that a person does not realize that he or she has an infection. Years later, when there is a recurrence of HSV, it may be mistaken for an initial attack, leading to unfair accusations about the source of infection.
For more information on STDs or to set up a consultation, click here. Thank you and we look forward to helping you.